A recent Innovad feed and blood survey identified mycotoxin risk in all the studied farms (> 800) and more than 50% of them were co-exposed to six or more mycotoxins. The deleterious effects of mycotoxins on different systems and organs such as the liver or the reproductive system have been described in detail, while the impact on the intestine has hardly been discussed. However, the gastrointestinal tract (GIT), as a filter against harmful toxins, is particularly affected by mycotoxins that alter intestinal integrity, modify absorption and digestion process, modulate immune responses, and change the microbiome (Figure 1).
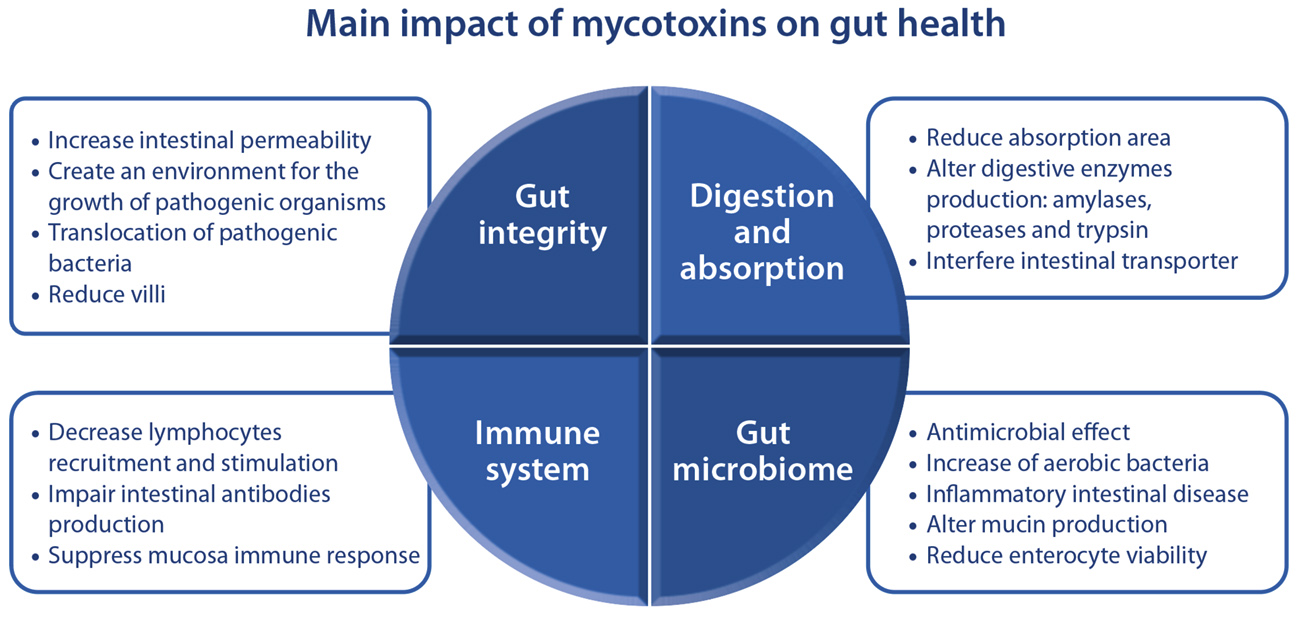
Figure 1. Mycotoxins have a big impact on the gut health: reducing gut integrity, decreasing digestion and absorption, altering the immune system and changing the gut microbiome. The incessant presence of mycotoxins, even at very low levels, not linked to obvious adverse effect, has a high negative influence on the intestional balance decreasing performance.
Highlights:
-
Most mycotoxins aggravate intestinal permeability. Consequently, pathogenic microorganisms can cause further infections.
-
Digestion and absorption of nutrients are reduced as mycotoxins decrease intestinal surface and transporters and digestive enzymes production.
-
The presence of mycotoxins alters the intestinal immune system, increasing parasitic, bacterial and virus infections.
-
The gut microbiome is modified by mycotoxins and consequently intestinal inflammation can occur.
-
Mycotoxin mitigation strategies must be comprehensive technologies to reduce impact of mycotoxins on gut health. Animals consuming Escent ® improved gut integrity and inflammation was reduced.
Mycotoxins and intestinal integrity
The intestinal epithelium composes a selective barrier and mediates the transport of molecules (either across the cells or between the cells). Any damage leads to increased permeability of the layer resulting in intestinal disorders. Numerous studies have evaluated the impact of mycotoxins on intestinal integrity, concluding that, except for zearalenone, all legislated mycotoxins (particularly deoxynivalenol) cause a strong impact on the intestinal epithelium aggravating intestinal permeability. It is noteworthy to mention emerging mycotoxins such as enniatins or beauvericin (highly common in cereals) also increase the intestinal permeability, even at a greater level than deoxynivalenol. The enlarged permeability creates inflammation with subsequent oxidative stress, and leakage of plasma amino acids or proteins into the gut, creating an environment that favors the massive overgrowth of pathogenic bacteria such as Clostridium perfringens. On the other hand, increased intestinal permeability, in turn, favors the translocation of bacteria and is responsible for the entry of pathogenic bacteria. For this reason, many in vivo studies detected correlations between mycotoxin exposure and worsening translocation of pathogenic strains such as E. coli, Salmonella typhimurium and Salmonella enteritidis. Finally, mycotoxins also alter the morphology of the GIT and a strong reduction of the villi height has been commonly detected in duodenum and jejunum decreasing the area available for nutrient absorption.
Mycotoxins and absorption and digestion processes
Mycotoxin presence reduces digestion and absorption processes in animals. Firstly, reduction of the villi and necrotic lesions in the GIT caused by mycotoxins reduces absorption surface in the GIT. Thus, animals exposed to mycotoxins have a reduced dietary protein absorption and increased protein content in the intestinal lumen. Moreover, mycotoxins at low level, like deoxynivalenol, T-2 or ochratoxin A, interfere with intestinal transporters reducing molecules absorption. For example, glucose absorption is compromised with mycotoxin presence. Besides, exposure to trichothecenes also shrink water absorption inducing diarrhea episodes. Further, several studies reported a decreased digestibility of dry matter, gross energy and/or metabolizable energy, crude protein/amino acids, crude fat of animals after exposure to aflatoxins, fumonisins and deoxynivalenol at concentrations in compliance with the regulations. The impact on synthesis and activity of digestive enzymes as amylases, proteases and trypsin is the main reason for the digestibility reduction.
Mycotoxins on intestinal defense
The GIT possesses its own immune system, and it is estimated that up to 70% of the immune defenses of the animal are in the intestine. Mycotoxins can also alter the intestinal immune system and cause immune dysfunction. On the one hand, lymphocytes recruitment and stimulation are reduced by mycotoxins, and it delays the response to parasitic infection as Eimeria. For this reason, there are correlations between exposure to mycotoxins and a higher impact of coccidiosis, even under the application of coccidiostat solutions. On the other hand, mycotoxins as fumonisins and deoxynivalenol demonstrated the capacity to impair the production of intestinal antibodies (Ig) and facilitate the colonization of pathogenic bacterial strains. Enteric virus can also have a greater impact under mycotoxin presence. Mycotoxins as deoxynivalenol or T-2 suppress the mucosal immune response, besides, they increase fecal excretion of virus favoring its dissemination. Finally, mycotoxins also modulate the inflammatory response: low doses upregulate the inflammatory response while high mycotoxin doses lead to the opposite profile by downregulating.
Mycotoxins and gut microbiome
The microbiota plays a crucial part in the health of the host, since it modulates many actions like the immune response, the synthesis of vitamins and the digestion of dietary fiber, as well as protecting against the colonization of pathogens. Therefore, the toxicity caused by mycotoxins in the gut microbiome can have dramatic effects on the host. Aflatoxin B1, enniatins, beauvericin and mycophenolic are well known for their strong antimicrobial effect that reduces the microbiome. Conversely, lower or no antimicrobial activity mycotoxins change the composition of the microbial community by increasing the presence of aerobic bacteria while anaerobic bacteria families as Enterobacteriaceae, Ruminococcaceae, Lachnospiraceae, Clostridiaceae, Lactobacillae and Veillonellaceae are reduced. The major presence of aerobic bacteria induce the vicious circle towards inflammatory intestinal diseases and alter the mucin production and enterocyte viability.
Mitigation of mycotoxin impact on the GIT
Compared to the limited distribution of mycotoxins in systemic tissues, the GIT is continuously facing the presence of mycotoxins. For this reason, the negative influence of mycotoxins on the intestinal balance is observed even at very low levels that are not linked to obvious adverse effects. The incessant presence of mycotoxins in the GIT causes a significant increase in maintenance requirements like repair of damaged tissues, maintenance of the integrity of the GIT, as well as metabolic cost associated with the stimulation of the immune system. For all these reasons, an effective mycotoxin mitigation strategy must be a comprehensive technology capable of supporting the GIT by improving gut integrity, absorption and digestion, immune response and beneficial microbiota.
Escent® combines different modes of action to alleviate the impact of mycotoxins on the GIT as demonstrated by several in vivo studies. Recently, Escent® was reported to improve GIT in broilers compared to the control group after chronic mycotoxin exposure throughout the cycle. For example, intestinal integrity biomarkers as OCLN (occluden proteins) and CLND (claudin proteins), both critical components of tight junctions, were improved in animals under Escent® (p<0.5). In addition, the inflammatory response was controlled thanks to Escent® as biomarker of inflammation, tumor necrosis factor alpha (TNF-α), was lower in animals that consumed Escent® (p<0.05) (Figure 2). All these positive effects provided by Escent® to GIT translated into better performance, since statistically significant improvements in weight gain and FCR were demonstrated, confirming the importance of supporting the GIT to improve final performance.
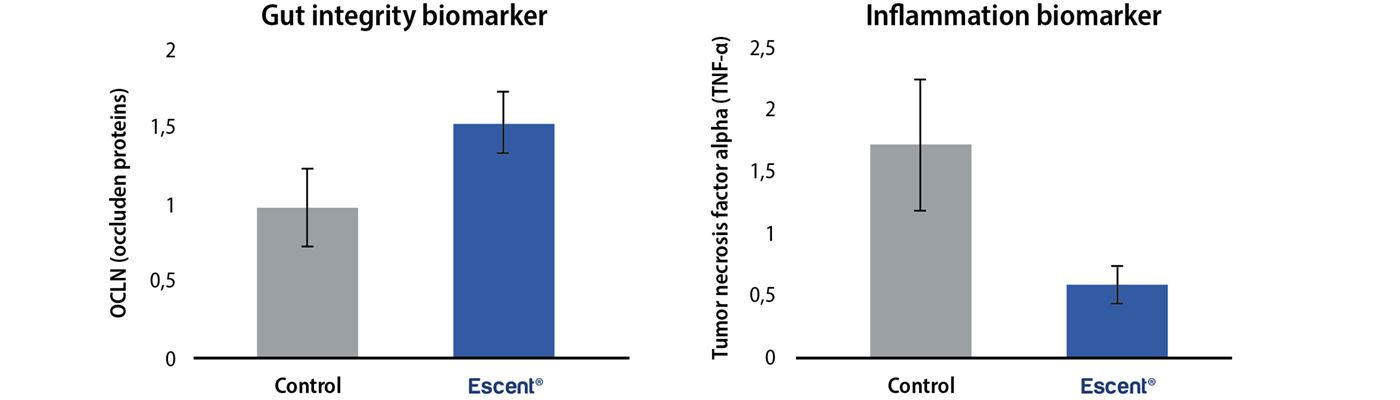
Figure 2. Gut integrity (occluden proteins) and inflammation (tumor necrosis factor alpha) biomarkers from the control and Escent® group demonstrating that animals (broilers) consuming Escent® had a better gut integrity and lower inflammation.
We can conclude that exposure to mycotoxins, even at low, ‘safe’ levels, has a big impact on animal health and chronic exposure results in reduced flock performance and economic losses. Innovad therefore regularly organizes classroom and practical sessions from top academics and field experts around the world on mycotoxin management, gut health and coccidiosis. We discuss how the different issues connect together to impact your animal’s performance and how to prevent and solve them. Join now and learn how mycotoxins, bacteriosis and coccidiosis connect together and impact performance at Innovad’s MBC Masterclasses.